Neurotransmitter imbalances in Obsessive Compulsive Disorder (OCD) – Comprehensive Overview:
Obsessive-Compulsive Disorder (OCD) is a mental health condition Caused by Neurotransmitter imbalances (chemical messengers), particularly Serotonin, Dopamine, and Glutamate. These imbalances disrupt brain circuits responsible for managing intrusive thoughts and compulsive behaviors, making it difficult to resist or suppress them. Below, we explore OCD symptoms, aetiology/causes, & evidence based treatment strategies in treating the OCD symptoms effectiveley.

Neurotransmitter imbalances in OCD- Seratonin production and Action
What Are Obsessions?
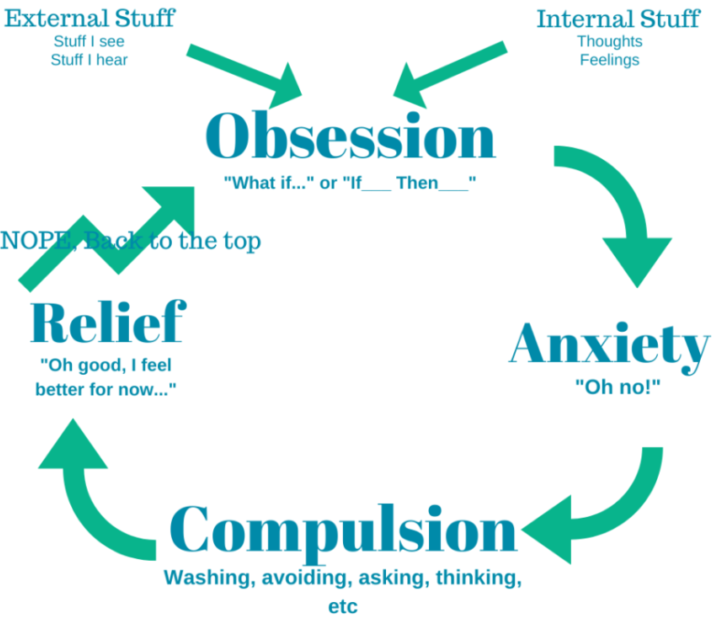
Obsessions are intrusive, unwanted thoughts, urges, or images that trigger significant anxiety or distress. Key features include:
- Recurrent and persistent thoughts or images: These occur repeatedly and are often experienced as disturbing.
- Efforts to suppress or neutralize obsessions: Individuals may try to counteract these thoughts through mental or physical actions.
What Are Compulsions?
Compulsions are repetitive behaviors or mental actions performed to relieve anxiety caused by obsessions. They include:
- Repetitive actions: Such as hand washing, checking, or arranging objects.
- Mental acts: Including counting, praying, or repeating words silently.
These actions are often excessive and disconnected from realistic outcomes, though they temporarily reduce anxiety.
The Impact Neurotransmitter imbalances in OCD in day to day life
OCD symptoms can consume a significant portion of a person’s day, leading to:
- Impaired daily functioning: Difficulty managing work, school, or relationships.
- Heightened stress levels: Persistent anxiety due to obsessive thoughts and the compulsion to act.
Prevalence of Neurotransmitter imbalances in OCD and Onset of OCD
- 12-Month Prevalence: 1.2% of the U.S. population, with slightly higher rates in females (except in childhood).
- Age of Onset:
- Average onset is 19.5 years.
- Males are more likely to have childhood onset.
Risk and Prognostic Factors
- Temperamental: High negative emotionality and childhood behavioral inhibition.
- Environmental: Early life trauma, such as abuse, increases susceptibility.
- Genetic and Neurobiological:
- A strong familial link exists, particularly for childhood-onset OCD.
- Neuroimaging studies reveal structural and functional abnormalities in brain regions linked to the CSTC circuit, highlighting the impact of neurotransmitter imbalances in Obsessive-Compulsive Disorder (OCD).
- Prognosis: While OCD is often chronic without treatment, early intervention, especially when tailored to address neurotransmitter imbalances in Obsessive-Compulsive Disorder (OCD), can lead to significant symptom reduction and improved quality of life
Key Points on Biological and Genetic Insights into OCD
Heterogeneous Etiology:
- OCD’s clinical diversity suggests multiple biological pathways for different subtypes.
Neurotransmitter Imbalances in Obsessive-Compulsive Disorder (OCD)
Emerging evidence points to abnormalities in neurotransmitter systems, including serotonin, dopamine, and glutamate, as significant contributors to OCD.
Serotonin Dysregulation:
- A deficiency in serotonin signaling is one of the most studied aspects of OCD. This imbalance is thought to influence the brain circuits involved in regulating repetitive behaviors and intrusive thoughts.
- The efficacy of selective serotonin reuptake inhibitors (SSRIs) highlights the role of serotonin in alleviating OCD symptoms.
Dopamine Dysfunction:
- Excess dopamine activity, particularly in the basal ganglia, has been linked to compulsive behaviors seen in OCD.
- This imbalance may also explain the overlap between OCD and tic disorders.
Glutamate Abnormalities:
- Dysregulated glutamate levels in the cortico-striato-thalamo-cortical (CSTC) circuit, a neural pathway critical for habit formation and error correction, are associated with OCD.
Understanding these imbalances provides a foundation for targeted therapies, such as glutamate-modulating medications, which are currently under investigation.
Animal Models:
- Naturally occurring OCD-like behaviors, such as canine acral lick in dogs and feather-picking disorder in birds, have been treated successfully with SSRIs, indicating similar underlying mechanisms.
Brain Imaging Studies:
- Abnormal hyperactivity in specific brain regions, such as the orbital frontal cortex, cingulate cortex, and head of the caudate nucleus, has been identified in OCD patients.
- Successful OCD treatment normalizes these metabolic abnormalities, supporting the theory of a hyperfunctioning brain circuit in OCD.
- Brain metabolism patterns may predict whether a patient responds better to SSRIs or CBT.
Neurological Hypothesis:
- OCD may be a neurologic disorder involving a hyperactive circuit in the frontal lobe and basal ganglia.
- Neurosurgical techniques targeting this circuit are often effective.
- SSRIs may work by desensitizing terminal 5-HT autoreceptors in the orbital frontal cortex, enhancing serotonin transmission.
Cognitive Dysfunction:
- Specific impairments in nonverbal memory, visuospatial skills, and visual attention have been identified in OCD patients.
- These deficits are linked to the structural abnormalities found in OCD-related brain regions.
Genetic Factors:
- Twin and family studies suggest a genetic predisposition to OCD, particularly for early-onset cases (before age 18).
- Familial aggregation is not typically observed in late-onset OCD cases.
- Specific polymorphisms in serotonin transporter and serotonin receptor genes (5-HT type 1Dβ and 5-HT type 2A) have been associated with OCD, but findings are inconsistent.
- Candidate genes, including catechol-O-methyltransferase, dopamine D4-receptor, and high-affinity neuronal/epithelial excitatory amino acid transporter, have shown potential links to OCD.
Research Implications:
- Continued investigation into structural brain abnormalities, genetic polymorphisms, and neurotransmitter functions is essential to develop targeted treatments for OCD.
Diagnostic Criteria for Neurotransmitter imbalances in OCD – DSM-5-TR criteria
A. Presence of Obsessions and/or Compulsions
- Obsessions: Persistent, intrusive thoughts, urges, or images that cause distress. These thoughts are often addressed through compulsive actions aimed at neutralizing anxiety.
- Compulsions: Repetitive behaviors or mental acts (e.g., checking, counting) performed in response to obsessions, often excessive and disproportionate to the perceived threat.
B. Time Consumption and Functional Impairment
Symptoms occupy more than one hour per day or cause significant disruption to social, occupational, or other areas of functioning.
C. Exclusion of Medical or Substance Causes
Symptoms are not attributable to substance use or another medical condition.
D. Differential Diagnosis
The symptoms cannot be better explained by other mental health disorders such as generalized anxiety disorder or body dysmorphic disorder.
It is vital to differentiate OCD from other mental health disorders, including:
- Generalized Anxiety Disorder (GAD): Focused on excessive worrying.
- Body Dysmorphic Disorder (BDD): Preoccupation with perceived flaws in appearance.
- Hoarding Disorder: Difficulty discarding possessions due to emotional attachment.
Additionally, OCD should not be confused with conditions like trichotillomania (hair pulling), excoriation (skin picking), or repetitive patterns seen in autism spectrum disorders.
Evidence-Based Treatment Approaches for Neurotransmitter imbalances in OCD
1. Cognitive-Behavioral Therapy (CBT)
Overview
CBT, particularly Exposure and Response Prevention (ERP), remains the cornerstone of OCD management.
Mechanism
- Encourages patients to face anxiety-provoking stimuli without engaging in compulsions.
Pediatric Application
- First-Line Treatment: Effective for children and adolescents.
- Adaptable Approaches: Tailored to developmental needs, with a focus on sustaining motivation for engagement.
2. Pharmacologic Interventions for Neurotransmitter imbalances in OCD
General Treatment Approaches
- Both medications and behavioral therapy effectively treat OCD.
- Combining medication with behavioral therapy offers optimal treatment outcomes.
Medications for OCD

CLASIFICATION of ANTIDEPRESSANTS
SSRIs
- Mechanism: Inhibit serotonin reuptake to manage OCD symptoms.
- FDA Approval: Effective options include fluvoxamine, fluoxetine, paroxetine, and sertraline.
- Approved for adults; all except paroxetine are also indicated for children.
- Efficacy: Meta-analyses reveal medium to large effect sizes, significantly better than placebo.
- Dosage: Maintain recommended SSRI dosage for at least four weeks before considering increases.
Venlafaxine
- An SNRI that is effective and better tolerated than clomipramine.
Clomipramine
Overview
- First Proven Drug: Effective in 60–70% of patients.
- MOA: A tricyclic antidepressant that acts as a potent serotonin reuptake inhibitor (SRI).
Use in Treatment
- Reserved for patients who fail at least two SSRI trials, consistent with guidelines.
- Requires careful monitoring due to a high overdose risk, especially in patients with comorbid depression.
Dosage and Administration
- Start: 25–50 mg/day, titrating to 150–200 mg/day over 2–4 weeks based on tolerability.
- Maximum dose: 250 mg/day (higher doses significantly increase seizure risk).
- Once-daily dosing is suitable after titration due to its 24-hour half-life.
Side Effects and Monitoring
- Common Side Effects: Sedation, dry mouth, dizziness, tremor, constipation, nausea (often subsiding with time).
- Long-Term Effects: Weight gain, sexual dysfunction, and rare liver enzyme elevation.
- Precautions:
- Perform ECG for cardiac risk evaluation before starting.
- Monitor liver function during the initial three months.
- Educate on avoiding alcohol and exercising caution during activities like driving.
Patient-Specific Considerations
- Asian Populations: May require lower doses due to decreased clearance.
- Genetic Polymorphisms: CYP2D6 poor or ultra-rapid metabolizers may need adjusted dosing or plasma level monitoring.
3. Treatment Considerations for Neurotransmitter imbalances in OCD- Children
MHRA Guidance
- Caution with SSRIs due to a modest rise in suicidal ideation.
- Benefits in pediatric OCD outweigh risks when closely monitored.
Challenges with CBT
- Developmental Barriers: Children with disabilities or low insight may find ERP overwhelming.
- Medication-Only Approach: Necessary when CBT is not viable.
Tailored Approaches
- Adjust treatments to account for comorbid conditions (e.g., ADHD, autism) that may affect engagement and outcomes.
Treatment Refractory OCD – Neurotransmitter imbalances in OCD
Augmentation Strategies
- Applied for partial responders to SSRIs or clomipramine.
- Antipsychotics:
- Second-Generation: Risperidone, olanzapine, and quetiapine are effective, with risperidone showing the most promise.
- Older Options: Haloperidol and pimozide are less favored due to side effects.
- Other Medications:
- Clonazepam: Occasionally effective as adjunctive or monotherapy, though benzodiazepines are generally not beneficial.
- MAOIs (e.g., phenelzine): Initial favorable results not supported by recent findings.
- SNRIs (e.g., duloxetine): Require further study.
Important Considerations
- Balance efficacy, tolerability, and patient-specific factors (e.g., comorbidities, prior responses).
- Behavioral therapy should remain central, with medications supporting resistant cases or where therapy access is limited.
- NICE Recommendations: Advocate for 3-month treatment trials at the maximum tolerated dose.
Up to 25% of pediatric patients may not respond to initial SSRI and CBT combinations. Options include:
- Switching SSRIs: Evidence suggests 40% may respond to a second SSRI.
- Augmentation Strategies:
- Adding low-dose risperidone for severe, resistant cases.
- Implementing clomipramine as a second-line agent.
- Specialist Referral: For complex cases, involving specialized centers improves care outcomes.

Management of Treatment Refractory OCD
Neurotransmitter imbalances in OCD- Augmentation Strategies
- Partial Response to Clomipramine:
- Augmenting clomipramine with an additional agent is common after 10 weeks if partial response is observed.
- SSRIs:
- Adding an SSRI (e.g., fluvoxamine, fluoxetine, paroxetine, sertraline) is an option but requires caution due to potential drug interactions via CYP450 pathways, especially CYP2D6.
- Citalopram and escitalopram: Preferred for minimal interaction risks, though evidence for efficacy as augmenting agents is limited.
- Second-Generation Antipsychotics:
- Risperidone (2 mg/day): Most effective and well-tolerated based on meta-analyses.
- Olanzapine and quetiapine: Alternatives, though with less supporting evidence compared to risperidone.
- Avoid first-generation antipsychotics (e.g., haloperidol) due to side effects and interactions.
Therapeutic Drug Monitoring (TDM):
- Monitor clomipramine and metabolite levels to adjust therapy effectively.
- High ratios of N-desmethylclomipramine to clomipramine may indicate poor clinical response and need for dose adjustment.
Guidelines and Long-Term Care for Neurotransmitter imbalances in OCD
NICE Stepped Care Model:
- Treatment intensity is adjusted based on the severity of OCD.
- Emphasis on continuous monitoring using tools like the Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS).
Relapse Prevention:
- Duration of Treatment: Maintain medication for at least six months post-remission to reduce relapse risks.
- Gradual Discontinuation: Abrupt cessation is discouraged to avoid symptomatic recurrence.
- Maintenance Strategies:
- Regular follow-ups and booster CBT sessions.
- Tailored support for individuals with developmental disabilities to enhance generalization of therapy outcomes.
Landmark OCD Clinical Trials and Key Findings- Neurotransmitter imbalances in OCD
1. Clomipramine Efficacy Trials (1980s)
Focus:
- Demonstrated the efficacy of clomipramine (a tricyclic antidepressant) over placebo in reducing OCD symptoms.
Key Findings:
- Clomipramine significantly improved OCD symptoms compared to placebo.
- This trial led to the widespread adoption of serotonergic agents for OCD treatment.
2. SSRI Trials (1990s)
Medications Studied:
- Fluoxetine, Fluvoxamine, Sertraline, and Paroxetine.
Focus:
- Evaluated the effectiveness of selective serotonin reuptake inhibitors (SSRIs) for OCD.
Key Findings:
- SSRIs consistently reduced OCD symptoms by addressing serotonin dysregulation.
- They became the first-line pharmacological treatment for OCD.
3. CBT vs. Medications (POTS Study, 2004)
Study Name:
- Pediatric OCD Treatment Study (POTS).
Focus:
- Compared cognitive-behavioral therapy (CBT), SSRIs, and their combination in pediatric OCD.
Key Findings:
- Combined therapy (CBT + SSRIs) was the most effective approach.
- CBT alone outperformed SSRIs alone, highlighting the importance of therapy in OCD treatment.
4. Deep Brain Stimulation (DBS) Trials (2010s)
Focus:
- Investigated the efficacy of DBS for treatment-resistant OCD.
Key Findings:
- Targeting brain areas like the subthalamic nucleus and ventral capsule/ventral striatum significantly reduced symptoms.
- FDA approved DBS for severe OCD under a Humanitarian Device Exemption.
5. Exposure and Response Prevention (ERP) Studies
Focus:
- Validated the efficacy of ERP, a specific CBT technique, for OCD.
Key Findings:
- ERP significantly reduced symptoms and improved quality of life.
- It often outperformed medication alone.
6. Serotonin Partial Receptor Agonists (SPRI-OB Trials, Recent)
Focus:
- Examined the role of serotonin partial receptor agonists in OCD treatment.
Key Findings:
- These agents showed promise, particularly in cases resistant to standard SSRIs.
7. Ketamine Infusion Therapy
Key Findings:
- Low-dose ketamine infusions provided rapid symptom relief compared to placebo.
- Benefits were temporary, offering potential for short-term symptom relief and opening avenues for studying glutamatergic modulation in OCD.
8. Transcranial Magnetic Stimulation (TMS) with CBT in Youth
Key Findings:
- Combining TMS with CBT improved symptom reduction in individuals aged 12–21.
- TMS showed potential as a non-invasive neuromodulation therapy for younger populations.
- The combination emphasized the value of integrating brain stimulation with psychotherapy.
9. QIMR Berghofer Brain Stimulation Trial
Key Findings:
- Mixed results highlighted challenges in achieving consistent outcomes with brain stimulation.
- Provided insights into the need for refined methods and patient-specific approaches in OCD treatment.
10. Enhanced Exposure and Response Prevention (ERP) in Youth
Key Findings:
- ERP alone or combined with SSRIs was more effective than SSRIs alone.
- Especially effective in reducing avoidance behaviors in youth.
- Reinforced the critical role of psychological therapies in OCD management.
11. Augmentation of SSRIs with Glutamate Modulators
Key Findings:
- Glutamate modulators (e.g., riluzole, memantine) provided modest benefits when added to SSRIs in treatment-resistant OCD.
- Highlighted glutamate dysregulation as a potential therapeutic target.
Conclusion
Obsessive-Compulsive Disorder (OCD) is a chronic condition requiring a multimodal approach combining CBT and pharmacotherapy. While SSRIs are the mainstay of drug treatment, individualizing interventions based on patient age, co-morbidities, and response to therapy ensures better outcomes.
Long-term follow-up, family involvement, and accessible care are essential to managing OCD and mitigating its profound impact on quality of life. Adhering to guidelines, such as those provided by NICE, equips clinicians with evidence-based tools to effectively combat this disorder.

3 Comments