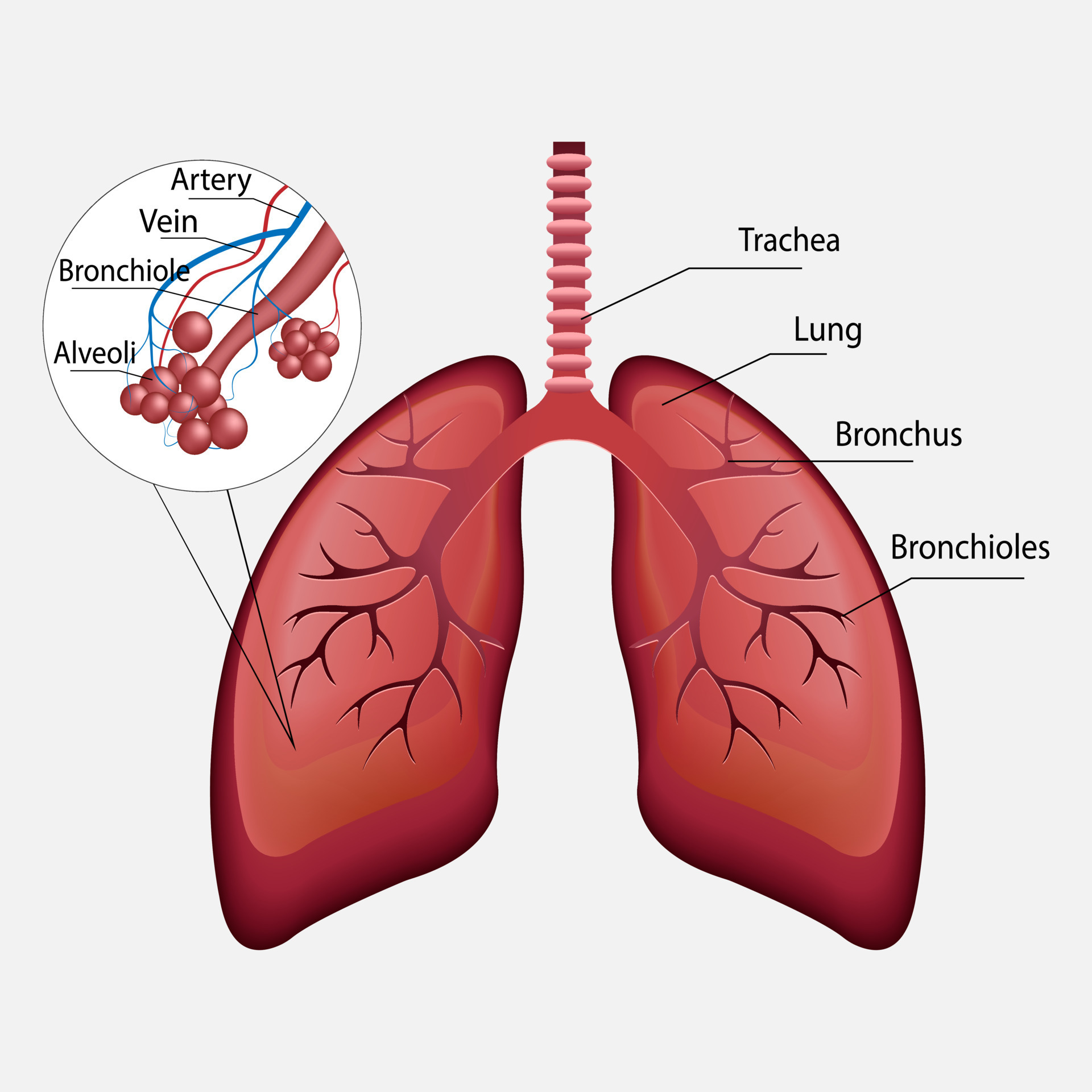
Upper respiratory tract infections (URTIs) are common, affecting areas like the nose, throat, pharynx, larynx, and bronchi. This guide explores Upper Respiratory Tract Infections and treatments, covering symptoms, diagnosis methods, and a range of treatment options, from medications to home remedies. These infections are widespread and can lead to significant discomfort and economic impact.
Understanding URTIS
URTIs can range from minor colds to more severe cases, with viral and bacterial infections affecting the respiratory tract. Common conditions include colds, influenza, sinusitis, pharyngitis, laryngitis, and bronchitis. Here’s a closer look at the specific conditions and treatments for managing URTIs.
Key Conditions and Symptoms
Allergic Rhinitis (Common Cold):
- Aetiology: Typically viral, triggered by pathogens like rhinovirus, influenza, or coronaviruses.
- Clinical Manifestations: Sore throat, runny nose, nasal congestion, and sometimes fever. COVID-19 may present specific symptoms like a sudden loss of smell or taste.
- Diagnosis: Generally based on symptoms, though COVID-19 testing may be necessary in relevant cases.
- Treatment Options: Over-the-counter pain relievers can treat sore throats and fevers. Decongestants and antihistamines also help ease nasal symptoms.
Common Nasal Decongestants: 
- Phenylephrine – (Eg: Dristan)
- Xylometazoline – (Eg: Otrivin / Otrivine / NozAIR)
- Oxymetazoline – (Eg: Nasivion / Afrin/ Sinarest)
- Naphazoline – (Eg: Privine / Otrivine)
- Pseudoephedrine – (Eg: Actifed / Sudafed)
- Phenylpropanolamine
Mechanism of Action (MOA):
(α2 agonists), specifically, naphazoline, xylometazoline, and oxymetazoline, produce local vasoconstriction when given topically in diluted solutions (0.05-0.1%).
Duration:
These drugs have a longer duration (up to 12 hours) than ephedrine and cause less after-congestion.
Side Effects:
- Initial stinging (particularly with naphazoline) and hazards with long-term use, such as reduced mucosal ciliary function, atrophic rhinitis, and anosmia, occur.
- Systemic Effects: CNS depression and a rise in blood pressure; caution is advised in hypertensives and patients on MAO inhibitors (selegiline, rasagiline, isocarboxazid).
Antihistamines (H1 Receptor Antagonists):
Antihistamines are medications that inhibit histamines in the body. They are often used to treat allergies, hay fever, and colds. There are 3 generations of antihistamines, each with varied efficacy and side effect profiles.
1st Generation Antihistamines (Sedating):
They cross the blood-brain barrier (BBB) and cause drowsiness.
- Diphenhydramine – (Benadryl or Nytol)
- Chlorpheniramine – (Piriton, Chlor-Trimeton, Hayleve, Cadistin)
- Promethazine – (Phenergan, Sominex)
- Clemastine – (Tavist)
- Pheniramine – (Avil)
- Cinnarizine – (Stugeron or Vertigon)
2nd Generation Antihistamines (Non-sedating):
Second-generation antihistamines are less likely to cause drowsiness, have minimal CNS depressant effects, and provide a longer duration of action.
- Cetirizine – (Zyrtec / Histazine / Cetzine)
- Loratadine – (Claritin / Clarityn / Alavert)
- Fexofenadine – (Telfast / Allegra / Altiva)
- Levocetirizine – (Xyzal or Levocet)
3rd Generation Antihistamines (Advanced Non-Sedating):
These are frequently selected for long-term allergy management.
- Desloratadine – (Aerius / Clarinex, Neoclarityn)
- Rupatadine – (Rupafin)
- Bilastine – (Bilaxten)
Mechanism of Action (MoA):
Antihistamines work by inhibiting histamine H1 receptors, easing symptoms such as sneezing, itching, and nasal congestion. First-generation antihistamines cross the blood-brain barrier and cause sedation, whereas second- and third-generation antihistamines are less likely to do so, reducing sleepiness.
Duration of Action:
- 1st-Gen Antihistamines: Typically lasts 4-6 hours and requires frequent dosing.
- 2nd-Gen Antihistamines: Longer duration of action (approx. 24 hours), allowing for once-daily dosing.
Systemic Effects and Counseling Points for Antihistamines:
- First-Generation Antihistamines: May cause CNS depression, impairing your ability to drive or operate machinery. Avoid mixing with alcohol or other sedatives.
- Second and Third-Generation Antihistamines: Generally safer but still exercise caution with alcohol. Fexofenadine may interact with fruit juices (e.g., grapefruit) and reduce its effectiveness.
Sinusitis:
- Aetiology: Bacterial (e.g., S. pneumoniae, H. influenzae, M. catarrhalis) or viral (e.g., rhinovirus, RSV).
- Clinical Manifestations: Acute cases last more than 10 days and may include fever and “double sickening.” Chronic cases persist for over 12 weeks and may involve nasal polyps and loss of smell.
- Diagnosis: Clinical evaluation; imaging or endoscopy may be necessary for chronic cases.
- Treatment: Antibiotics (e.g., amoxicillin-clavulanate) for bacterial infections, decongestants for symptom relief, and surgery for chronic cases.
Pharyngitis (Strep Throat):
- Aetiology: Bacterial (group A streptococcus) or viral (e.g., influenza, EBV).
- Clinical Manifestations: Bacterial pharyngitis includes sore throat, visible pus on the tonsils, and fever. Viral cases may also involve cough and runny nose.
- Diagnosis: Strep throat is confirmed with a rapid antigen test, with antibiotics prescribed for bacterial cases.
- Treatment: Antibiotics (e.g., amoxicillin-clavulanate) for bacterial infections, decongestants for symptom relief, and rest and fluids for viral cases.
CENTOR Score & Fever PAIN Score online Calculator
[centor_fever_calculator]
[fever_pain_calculator]
The Centor Score is used to assess the likelihood of streptococcal pharyngitis (strep throat):
- 0-1: Low likelihood of strep, no antibiotics needed.
- 2-3: Moderate likelihood, consider a rapid strep test or culture.
- 4-5: High likelihood of strep, antibiotics should be considered.
A higher score indicates a greater probability of strep throat, guiding treatment decisions.
Fever Pain Score Interpretation:
- 1–4: Mild condition.
- 5–8: Moderate condition.
- 9–12: Severe condition.
A higher score indicates greater severity of fever, pain, and fatigue, potentially requiring medical attention.
Clinical Prediction Scores for Streptococcal Infections
| Criteria | CENTOR Score | Fever PAIN Score |
| C – Absence of cough, coryza, conjunctivitis | +1 | +1 |
| E – Exudate from tonsils | +1 | +1 |
| N – Swollen/painful anterior cervical lymph nodes | +1 | +1 |
| T – Temperature >38°C | +1 | +1 |
| Age | ||
| 3-14 Years | +1 | +1 |
| 15-44 Years | 0 | 0 |
| >45 Years | -1 | -1 |
Interpretation:
| Score | CENTOR Score Interpretation | Fever PAIN Score Interpretation |
| 0 | 5-10% (Low probability) | 2-3% (Very low probability) |
| 1 | 10-17% (Low probability) | 4-6% (Low probability) |
| 2 | 30-35% (Moderate probability) | 10-12% (Moderate probability) |
| 3 | 50-60% (High probability) | 27-28% (High probability) |
| 4 | 70-80% (Very high probability) | 38-63% (Very high probability) |
| 5 | 90%+ (Very high probability) | N/A |
Natural Remedies for (Cold & Cough) Upper Respiratory Tract Infections
- Mix honey and turmeric for an easing nighttime cough and better sleep.
- Thyme and Ginger Steam: Inhale for effective sinus care and decongestion.
- Salt Water + Apple Cider Vinegar Gargle: Gargle to relieve throat irritation and fight infections.
- Drink Elderflower and Lemon Balm Tea to increase immunity and treat minor fevers.
- Massage garlic-infused olive oil onto your chest and sinuses for antimicrobial relief.
- Licorice and Marshmallow Root Tea: Consume to reduce congestion and soothe the throat.
- Cucumber-Citrus Infused Water: Stay hydrated with antioxidants that boost your immune system.
- Peppermint and Rosemary Vapor Rub: Apply to your chest to relieve congestion naturally.
- Probiotic Smoothie with Ginger and Berries: Blend to boost immunity and combat URTI symptoms.
- Elderberry and Clove Lozenges: Dissolve to boost immunity and soothe your throat.
- Turmeric and Black Pepper Paste: Take daily to reduce inflammation and boost your immunity.
FAQs in Upper Respiratory Tract Infections & Treatments
Q: What are the primary symptoms of Upper Respiratory Tract Infections?
A: Common symptoms include cough, sore throat, fever, nasal congestion, and shortness of breath.
Q: When should I see a doctor for a respiratory infection?
A: Seek medical advice if symptoms persist for more than a week, are severe, or if you have underlying health conditions.
Q: How can I differentiate between viral and bacterial infections?
A: Viral infections usually cause symptoms like a runny nose and cough, while bacterial infections may present with high fever and purulent discharge.
Final Thoughts on URTIs & Treatments
Upper respiratory tract infections are common, yet they can be disruptive. Thankfully, with a mix of traditional medications and natural remedies, you can effectively manage symptoms and support your immune system for quicker recovery.


1 comment so far