Introduction to Tolterodine and Urinary Incontinence Management
Urinary Incontinence -Tolterodine:
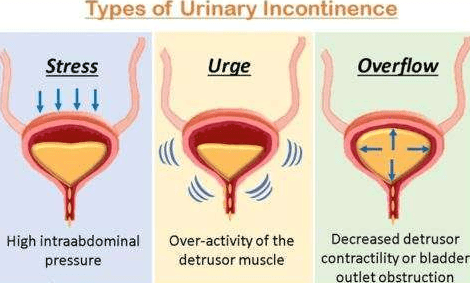
Tolterodine is a widely used antimuscarinic medication in the treatment of urinary incontinence, particularly in patients with overactive bladder (OAB). OAB is characterized by symptoms such as frequent urination, urgency, and involuntary leakage. Tolterodine works by targeting specific muscarinic(M3) receptors in the bladder, reducing muscle contractions, and helping patients regain control over urinary frequency and urgency. This profile covers Tolterodine’s effectiveness, potential side effects, and key safety considerations for its use in various patient populations.

Image Source: https://imagetou.com/my-img-anticholinergic-drugs-classification.html
Tolterodine Overview
Drug Category: Antimuscarinic (Anticholinergic)
Mechanism of Action: Blocks M3 muscarinic receptors, relaxing the bladder muscles
Indications: Overactive bladder with symptoms of urinary frequency, urgency, and urge incontinence
Major Side Effects: Dry mouth, constipation, blurred vision, drowsiness, urinary retention
Understanding Tolterodine as an M3 Receptor Antagonist
Chemical Structure:
- Molecular Formula: C₂₂H₃₁NO
Classification and Brands:
Tolterodine inhibits the detrusor muscle in the bladder. By blocking the muscarinic (M3) receptors in the detrusor muscle, Tolterodine helps relax this muscle, reducing involuntary contractions. This relaxation increases the bladder’s storage capacity, decreasing the urgency and frequency of urination associated with overactive bladder (OAB).

- Detrusitol
- Detrol
- Ditrax
- Tolterodine Actavis

- Toviaz
- Tovium
- Toltaren
- Tolaris
- Neditol
- Uro-Tol

Antimuscarinic Mnemonic for OAB Drugs
“STOP Frequent trips to the toilet”:
- S – Solifenacin

- T – Tolterodine, Trospium
- O – Oxybutynin
- P – Darifenacin
- F – Fesoterodine (Tolterodine’s prodrug)
Clinical Considerations for Tolterodine in Urinary Incontinence
1. Behavioral Therapy: As a first-line treatment for OAB, behavioral interventions like bladder training and pelvic exercises can be effective.
2. Antimuscarinic Therapy: Tolterodine and other antimuscarinic agents, especially in extended-release (ER) forms, are typically second-line treatments.
3. Population Suitability: Tolterodine’s selectivity for bladder M3 receptors, along with minimal CNS impact, makes it a preferred option for elderly patients due to a lower risk of cognitive side effects. Trospium, which does not cross the blood-brain barrier, is another favorable option for elderly patients.
The safety of the Tolterodine drug profile needs to be known in Special Populations
Tolterodine is commonly used to treat overactive bladder, but its safety varies in special populations. Here’s a simplified breakdown:
1. Elderly
- Considerations: Older adults may experience more anticholinergic side effects, like dry mouth, constipation, and cognitive issues. Age-related changes in the body can increase these risks.
- Dose Adjustments: Start with a lower dose (1 mg twice daily) and consider ER formulations for sustained effects and fewer side effects.
- References:
- Nitti VW, Urology. 2004
- Mader et al., Drugs & Aging. 2005
2. Hepatic Impairment
- Considerations: Tolterodine is processed by the liver, and liver problems can slow its breakdown. This may lead to higher drug levels and increased side effects.
- Dose Adjustments: Use half-dose for moderate to severe hepatic impairment; for severe cases, alternatives should be explored.
- References:
- Tolterodine [package insert]
- Nair et al., Journal of Clinical Pharmacology. 2002
3. Renal Impairment
- Considerations: Impaired kidney function can prolong drug clearance.
- Dose Adjustments: Dose reduction in severe renal impairment (creatinine clearance <30 mL/min) is recommended.
- References:
- Tolterodine [package insert]
- Rovner et al., BJU International. 2002
4. Pregnancy and Breastfeeding
Pregnancy and Breastfeeding
Pregnancy: Tolterodine is classified as Category C; risks may exist for the fetus, and it should only be used if the benefits outweigh the risks.
Breastfeeding: Since it passes into breast milk, alternative treatments are suggested.- References:
- Tolterodine [package insert]
- Hale, T. W. Medications and Mothers’ Milk. 2017
5. Pediatric Population
- Considerations: Limited data on safety and effectiveness in children; generally not recommended.
- References:
- Tolterodine [package insert]
- Green RL, et al., Journal of Urology. 2008
Conclusion
Tolterodine is generally safe in special populations when dose adjustments are made. It’s important to consider the patient’s age, liver, and kidney function, and other health conditions. Furthermore, always follow up with updated clinical guidelines and references to ensure the best care.
WHY Tolteridine ??
Dosage and Contraindications
Standard Dosage:
- Immediate-Release: 2 mg twice daily
- Extended-Release: 4 mg once daily
Contraindications:
Avoid in patients with:
- Angle-closure glaucoma
- Gastrointestinal obstruction or intestinal atony
- Myasthenia gravis (unless for counteracting muscarinic side effects)
- Toxic megacolon
- Urinary retention
- paralytic ileus or pyloric stenosis.
- severe ulcerative colitis or significant bladder outflow obstruction
Pharmacokinetics and Mechanism of Action (MOA) of Tolterodine
Upon oral administration, Tolterodine is well-absorbed and reaches peak concentration in 1-2 hours. It undergoes liver metabolism, mainly through the CYP2D6 enzyme, producing an active metabolite contributing to its effectiveness. It has a half-life of approximately 2-3 hours, with excretion via urine and feces.
Mechanism of Action of Tolterodine in Treating Urinary Incontinence
Tolterodine selectively inhibits muscarinic receptors (primarily M3) in the detrusor muscle of the bladder. This action decreases involuntary bladder contractions, allowing the bladder to store urine for longer, reducing both urgency and frequency of urination.
Indications for Tolterodine in Urinary Incontinence
Tolterodine is prescribed to manage symptoms associated with OAB, including frequent urination, urgency, and urge incontinence, particularly in patients who haven’t found success with lifestyle changes alone. It is highly effective for improving bladder control in cases of severe urinary incontinence.
Tolterodine Common and Rare Side Effects in Urinary Incontinence Treatment
- Common Side Effects:
- Dry Mouth: Manageable with hydration or sugar-free gum.
- Constipation: Increasing fiber and water intake is recommended.
- Blurred Vision and Dry Eyes: Patients with contact lenses should exercise caution.
- Drowsiness and Headache: Impacts activities requiring alertness; assess tolerance when driving.
- Urinary Retention: Particularly in those with a history of retention; consult healthcare providers beforehand.
- Rare Side Effects: Arrhythmia, heart failure, memory loss, and nervousness.
Landmark Clinical Trials for Tolterodine in the Treatment of Urinary Incontinence
TAURUS Study (Tolterodine As Urinary Regimen for Urinary Symptoms):
- Objective: The TAURUS study investigated the safety and efficacy of tolterodine in reducing OAB symptoms in adults.
- Findings: Results indicated that tolterodine significantly reduced frequency, urgency, and incontinence episodes, improving patient quality of life. This study established tolterodine as a reliable option for managing overactive bladder.
VANTAGE Study (Vesicare And Tolterodine In General Effectiveness):
- Objective: This study compared tolterodine to another antimuscarinic, assessing which was more effective for OAB symptom relief.
- Findings: Tolterodine showed comparable efficacy in symptom reduction but had a slightly lower incidence of dry mouth. This supported tolterodine’s effectiveness with fewer side effects, solidifying its place in OAB management.





Leave a Reply