Benign Prostatic Enlargement (BPE) : Causes, Symptoms & Treatment
Introduction:
Benign Prostatic Enlargement (BPE), also known as Benign Prostatic Hyperplasia (BPH), is a common condition among aging men. This non-cancerous growth of the prostate gland can cause various urinary symptoms that may affect daily life. Fortunately, understanding its causes, recognizing its symptoms, and exploring modern treatments can help men effectively manage this condition and maintain good prostate health.
Definition & Pathophysiology of Benign Prostatic Enlargement (BPE)
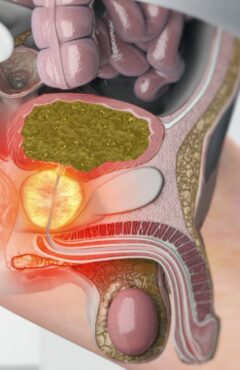
Benign Prostatic Enlargement (BPE) is a condition characterized by an increase in the size of the prostate gland. This condition is linked to changes in prostate tissue known as Benign Prostatic Hyperplasia (BPH), which commonly occurs as men age, It is characterized by the non-cancerous enlargement of the prostate gland, leading to lower urinary tract symptoms (LUTS). Common symptoms include difficulty in urination, frequent urination (especially at night, known as nocturia), and urinary retention. Effective treatment focuses on symptom relief, slowing disease progression, and improving quality of life through a combination of lifestyle changes and pharmacologic therapies.
How does BPE develop?
BPE typically begins in the peri-urethral (transitional) zone of the prostate, where the glandular and stromal tissues expand. However, the degree to which each tissue type is affected can vary.What triggers prostate growth?
On average, the prostate grows by 2.4 cm³ per year, starting around age 40. Although the exact cause of BPE is unknown, hormonal changes involving testosterone and dihydrotestosterone (DHT) are believed to play a significant role.What role do hormones play in Benign Prostatic Enlargement (BPE)?
- Hormones appear to be crucial, as BPE does not occur in men with low testosterone levels (hypogonadism). This suggests that both testosterone and its derivative, DHT, are central to the development of BPE.

The pituitary-gonadal axis regulates benign prostatic hyperplasia through endocrine mechanisms.
Flowchart: Understanding the Causes of Benign Prostatic Enlargement (BPH)
Key Factors Leading to BPH
Hormonal Processes
Aging Processes
⬇️
Essential Condition for BPH Development
Presence of intact, normally functioning testes.
Castration before puberty prevents BPH development.
⬇️
Role of Androgens in the Prostate
Testosterone is the major circulating androgen.
Testosterone is metabolized into Dihydrotestosterone (DHT) by the enzyme 5α-reductase.
⬇️
5α-Reductase Isoenzymes
Type 1: Found throughout the body and in the prostate.
Type 2: Found predominantly in the prostate and other genital tissues.
⬇️
Importance of DHT in Prostate Growth
DHT is the active androgen responsible for:
RNA synthesis
Protein synthesis
Cell replication
⬇️
Potential Role of Testosterone
Testosterone may initiate fibroadenomatous hyperplasia leading to glandular enlargement.
Who is affected?
By age 60, over half of men may experience symptoms of prostate enlargement, including difficulties with urination due to urethral compression.What are the consequences of BPE?
While the enlargement is non-cancerous, it can exert pressure on the urethra, leading to urinary symptoms such as- a weak stream
- frequent urination
- difficulty starting or stopping urination.
Understanding the differences between urinary incontinence, stress incontinence, urinary retention, and related terms is essential for identifying and managing urinary issues effectively. Here’s a breakdown of these conditions:
What is Stress Incontinence ?
What is Urinary Retention ?
Urinary Retention
What is Overactive Bladder (OAB)? Nocturia? Dysuria? Hematuria ?
Overactive Bladder (OAB)
Nocturia
Dysuria
Hematuria
Key Differences at a Glance
| Condition | Main Feature | Trigger or Cause | Key Symptom |
| Urinary Incontinence | Involuntary urine leakage | Weak bladder control, nerve damage | Leakage during daily activities |
| Stress Incontinence | Leakage with physical activity | Increased abdominal pressure, weak muscles | Leakage during sneezing, coughing, etc. |
| Urinary Retention | Inability to empty bladder fully | Obstruction, nerve damage | Difficulty starting or weak stream |
| Overactive Bladder | Sudden urge to urinate | Overactive bladder muscles | Frequent, urgent urination |
| Nocturia | Frequent nighttime urination | Aging, prostate issues, or diabetes | Disrupted sleep due to urination |
| Dysuria | Pain during urination | UTIs, stones, or irritation | Burning or discomfort when urinating |
Prostate Gland Enlargement (BPH) Symptoms:
Men with BPH often experience a range of prostate issues, many of which are associated with changes in urinary habits. Common symptoms include:
- Difficulty urinating: This includes hesitancy, a weak urine stream, or straining to urinate.
- Frequent urination at night (nocturia): Waking up multiple times to urinate disrupts sleep.
- Incomplete bladder emptying: A sensation that the bladder is not fully emptied after urination.
- Urgency and leakage: Sudden, strong urges to urinate can lead to accidents.
These symptoms are collectively referred to as lower urinary tract symptoms (LUTS). While they are not life-threatening, they can lead to significant distress if untreated.
Diagnosis of Benign Prostatic Hyperplasia (BPH)
The Boyarsky Index and the International Prostate Symptom Score (IPSS) are both tools designed to assess urinary symptoms, but they are not the same. Below is a detailed explanation of each system, their features, and how they differ.
What Is the Boyarsky Index?
The Boyarsky Index is an older system used to evaluate urinary symptoms, particularly those associated with benign prostatic hyperplasia (BPH). It categorizes symptoms into two main types:
Obstructive symptoms: These include:
- Difficulty starting urination.
- A weak or interrupted urine stream.
- A feeling of incomplete bladder emptying.
Irritative symptoms: These include:
- Frequent urination (increased daytime frequency).
- A sudden, strong urge to urinate (urgency).
- Waking up multiple times at night to urinate (nocturia).
While the Boyarsky Index was beneficial in the past, it is now considered outdated and is less commonly used. Modern tools, like the IPSS, offer a more standardized and comprehensive approach.
International Prostate Symptom Score
The IPSS is a generally acknowledged and standardized questionnaire developed by the American Urological Association. It is used extensively to measure lower urinary tract symptoms (LUTS), particularly in men with BPH. IPSS is an eight-question written screening instrument designed to detect, quickly diagnose, track, and recommend treatment for the symptoms of BPH
“FINDING WAYS To Wee”
This mnemonic helps you recall the eight key symptoms that the IPSS (International Prostate Symptom Score) assesses:
- F – Frequency (How often you urinate during the day)
- I – Incomplete emptying (Feeling like you can’t fully empty your bladder)
- N – Nocturia (Waking up at night to urinate)
- D – Difficulty starting urination (Intermittency or hesitation)
- I – Intermittency (The stream of urine starts and stops)
- N – Need to Urinate Urgently (Urgency)
- G – Grade of Stream (Weak stream or reduced urine flow)
- W – Weak Stream (A weak or slow flow of urine)
- A – Abdominal Straining (Straining to urinate)
- Y – You’re not feeling complete (Feeling of incomplete emptying)
- S – Satisfaction (Quality of life with urinary symptoms)
- To Wee – Toileting interference (Symptoms interfering with daily life, lifestyle changes)
Is the Boyarsky Index the Same as the IPSS?
Key Features of the IPSS:
It consists of 7 questions that address both obstructive and irritative symptoms. Each question is scored from 0 to 5, with higher scores indicating more severe symptoms.
- Obstructive symptoms: Difficulty emptying the bladder, intermittent urine flow, weak stream, and straining during urination.
- Irritative symptoms: Urgency, increased frequency of urination, and nocturia.
An optional 8th question evaluates the impact of symptoms on the patient’s quality of life.
The total score ranges from 0 to 35, with categories for severity:
- 0–7: Mild symptoms.
- 8–19: Moderate symptoms.
- 20–35: Severe symptoms.
Online I-PSS calculator / Assess Your Prostate Health Today

Take the IPSS questionnaire today to assess the severity of your symptoms.
The IPSS is now the gold standard for assessing LUTS in BPH due to its reliability and ease of use.
Comparing the Boyarsky Index and IPSS
| Aspect | Boyarsky Index | IPSS |
| Origin | Older, less frequently used system. | Developed by the AUA, globally recognized. |
| Symptoms Addressed | Focuses on obstructive and irritative symptoms. | Covers obstructive/irritative symptoms and quality of life. |
| Questions | Categorized symptoms without a standard scale. | 7 questions (scored 0–5) + 1 optional quality-of-life question. |
| Scoring Range | No universal scoring range or categories. | 0–35 (mild, moderate, or severe symptoms). |
| Relevance Today | Rarely used in clinical practice. | Considered the gold standard for LUTS assessment. |
Why the IPSS is Superior
While the Boyarsky Index was a useful tool in its time, it lacks the standardization and global acceptance of the IPSS. The IPSS not only evaluates symptoms more thoroughly but also considers the patient’s quality of life, making it a more effective and practical choice for modern clinical practice.
Therapeutic Choices for Managing Benign Prostatic Enlargement (BPE)
Benign Prostatic Enlargement (BPE), also referred to as benign prostatic hyperplasia (BPH), is a common condition in aging men, characterized by prostate enlargement leading to lower urinary tract symptoms (LUTS). Effective management involves nonpharmacologic, pharmacologic, and combination therapy approaches. Here is a detailed guide to therapeutic options.
Nonpharmacologic Choices
For men with minimal symptoms, nonpharmacologic interventions focus on lifestyle modifications and regular monitoring:
- Active Surveillance: Reassure patients with mild symptoms and conduct regular reassessments.
- Lifestyle Adjustments:
- Advise reducing evening consumption of caffeine and alcohol, especially for those with nocturia.
- Encourage patients to maintain a healthy weight and stay physically active.
Phytotherapy: Certain plant-based agents may provide symptom relief, though their effectiveness varies.
Pharmacologic Choices for BPE(Benign Prostatic Enlargement)
Several effective pharmacologic treatments are available for managing BPE symptoms. These therapies include α1-adrenergic receptor antagonists, 5-alpha-reductase inhibitors, and combination therapies.
Alpha-1 Blockers for Benign Prostatic Enlargement
Alpha-1 blockers are a cornerstone in treating BPE by relaxing smooth muscles in the bladder neck, prostate, and urethra to relieve symptoms.
1. Prazosin (Minipress, Prazo, Prazopres, Vasoflex, Betradex)
- Mechanism: A non-selective alpha-1 blocker (α1:α2 ratio of 1000:1) that inhibits all α1 receptor subtypes (α1A, α1B, α1D).
- Benefits:
- Improves urinary flow and reduces residual urine volume.
- Has additional vasodilatory effects by inhibiting phosphodiesterase.
- Cautions: Known for the “first-dose effect,” causing postural hypotension; starting with low doses minimizes this risk.
2. Terazosin (Hytrin, Teralfa, Olyster, Traten, Zoxan)
- Features:
- Long-acting with a 12-hour half-life, allowing once-daily dosing.
- May promote prostate cell apoptosis, slowing BPE progression.
- Advantages: Effective for BPE symptoms and hypertension management.
- Side Effects: Orthostatic hypotension, dizziness—monitor during dose adjustments.
3. Doxazosin (Cardura, Doxacard, Doxapress, Duralin, Duracard, Doxamax, Uroxad)
- Highlights:
- A long-acting alpha-1 blocker with an 18-hour half-life.
- Similar to terazosin in efficacy and apoptosis-inducing effects.
- Benefits: Reliable for long-term control of both BPE symptoms and hypertension.
- Side Effects: Dizziness, syncope, and orthostatic hypotension, particularly at higher doses (>4 mg/day).
Uroselective Alpha-1 Blockers for BPE
Uroselective alpha-1 blockers target receptors primarily in the prostate and bladder, reducing systemic side effects.
1. Alfuzosin (Xatral, Alfusin, Uroxatral, Alfor)
- Selectivity: Non-selective for alpha-1 receptor subtypes but optimized for relieving lower urinary tract symptoms (LUTS) in BPE.
- Dosage: 10 mg extended-release (ER) daily, typically taken after meals.
- Interactions: CYP3A4 inhibitors (e.g., erythromycin) may require dose adjustments.
2. Tamsulosin (Flomax, Omnic, Urimax, Contiflo, Tamsol)
- Mechanism: Selective for alpha-1A/alpha-1D receptors, concentrating its effects on the prostate and bladder.
- Advantages:
- Minimal cardiovascular side effects like hypotension.
- Modified-release forms enable once-daily dosing.
- Cautions: Retrograde ejaculation and “floppy iris syndrome” in cataract surgery are notable side effects.
- Dosage: 0.4–0.8 mg daily, preferably after meals.
3. Silodosin
- Specificity: Highly selective for alpha-1A receptors in the prostate and bladder.
- Dosage: 8 mg/day, with adjustments for renal impairment.
- Considerations: High efficacy in symptom relief but with a higher incidence of retrograde ejaculation (~21%).
Mechanism of Action for Alpha-1 Blockers in BPE
Alpha-1 blockers directly address Benign Prostatic Enlargement symptoms by relaxing smooth muscle tone in the bladder neck, prostate, and urethra. This leads to:
- Faster relief of obstructive symptoms like hesitancy and dribbling, often noticeable within two weeks.
- Improvement in voiding symptoms, though they are less effective for irritative symptoms like urgency or frequency.
Combination Therapy in Benign Prostatic Enlargement
For optimal management of BPE, combination therapy involving alpha-1 blockers and 5-ARIs is often recommended.
Benefits of Combination Therapy
- Immediate Relief: Alpha-1 blockers quickly alleviate symptoms.
- Long-Term Control: 5-ARIs, such as finasteride or dutasteride, reduce prostate size and progression risks.
- Clinical Trials:
- MTOPS Trial: Demonstrated a 66% reduction in BPE progression with combination therapy.
- CombAT Trial: Highlighted superior symptom control and lower risks of acute urinary retention or surgery.
Example Combination
Dutasteride (0.5 mg) combined with tamsulosin (0.4 mg) in a single formulation improves adherence and efficacy.
Dosage Guidelines for Alpha-1 Blockers in BPE
- Prazosin: Start with 0.5–1 mg at bedtime; maintain at 1–4 mg twice or thrice daily.
- Terazosin: Begin with 1 mg/day and titrate to 2–10 mg/day as tolerated.
- Doxazosin: Start at 1 mg/day and increase up to 8 mg/day for persistent symptoms.
- Alfuzosin: 10 mg ER daily, taken post-meal to optimize absorption.
- Tamsulosin: 0.4–0.8 mg/day, usually after meals.
5-Alpha-Reductase Inhibitors (5-ARIs) for BPE
5-ARIs target the hormonal cause of prostate growth in Benign Prostatic Enlargement, offering a long-term solution.
Finasteride
- Mechanism: Blocks the type 2 isoenzyme of 5-alpha-reductase, reducing dihydrotestosterone (DHT) levels by 85%.
- Benefits:
- Decreases prostate size by ~24% within 12 months.
- Improves urinary flow rates (+2.9 mL/sec) and symptom scores.
- Side Effects: Mild sexual dysfunction, typically reversible after discontinuation.
Dutasteride
- Mechanism: Inhibits both type 1 and type 2 5-alpha-reductase isoenzymes, achieving a 90% reduction in DHT levels.
- Efficacy:
- Symptom relief within three months, particularly effective for prostates >30g.
- Side Effects: Similar to finasteride but with slightly higher risks of gynecomastia and reduced libido.
Key Considerations for Managing Benign Prostatic Enlargement
- Monitoring: Regular follow-ups to assess response and side effects, especially with alpha-1 blockers like prazosin, which carry a risk of postural hypotension.
- Combination Therapy: Ideal for patients with moderate-to-severe symptoms and enlarged prostates.
- Discontinuation: Alpha-1 blockers may be tapered after symptoms stabilize for six to twelve months.
- Patient Selection:
- Uroselective blockers like tamsulosin are suitable for those with cardiovascular risks.
- 5-ARIs are recommended for men with significantly enlarged prostates (>40g).
Imprortant Clinical Trails in Benign Prostatic Enlargement
The Medical Therapy of Prostatic Symptoms (MTOPS) Study
- Year: 2003
- Purpose: To evaluate the long-term effectiveness of combination therapy with α1-blockers (terazosin) and 5α-reductase inhibitors (finasteride) in patients with BPE.
- Key Findings:
- The study found that combination therapy (terazosin + finasteride) was more effective than either treatment alone in reducing symptoms of BPE, improving urinary flow, and reducing prostate volume.
- Finasteride alone slowed disease progression by decreasing prostate volume.
- Terazosin improved urinary symptoms and flow.
- Combination therapy significantly reduced acute urinary retention and the need for BPH-related surgery.
- Impact: This trial helped establish the benefit of combining α1-blockers with 5α-reductase inhibitors for better symptom management and disease progression in BPE.
2. The PRACTICAL Study (Prostate Cancer and Treatment Study)
- Year: 2014
- Purpose: To investigate whether the 5α-reductase inhibitor finasteride affects prostate cancer risk, with a secondary focus on BPH symptoms.
- Key Findings:
- While the primary goal was to assess prostate cancer risk, the trial showed that finasteride improved urinary symptoms in patients with BPE.
- Finasteride resulted in a decrease in prostate volume and improved urinary flow in patients with BPH.
- Impact: The study demonstrated the efficacy of finasteride in improving BPH symptoms, further supporting its role in BPE management, even though it had concerns about increasing the risk of high-grade prostate cancer.
3. The ALFIE Trial (Alfuzosin for Lower Urinary Tract Symptoms due to BPH)
- Year: 2003
- Purpose: To assess the effectiveness of alfuzosin, a α1-adrenergic blocker, in treating lower urinary tract symptoms (LUTS) due to BPH.
- Key Findings:
- Alfuzosin was shown to significantly improve symptoms of BPE such as urinary flow, urgency, and nocturia.
- It had a favorable side-effect profile, with fewer cardiovascular effects compared to other α1-blockers like terazosin.
- Impact: The ALFIE trial helped establish alfuzosin as an effective and well-tolerated option for managing BPH, with a favorable safety profile.
4. The COMBAT Study (Combination Therapy for BPH)
- Year: 2011
- Purpose: To compare the effects of combination therapy (α1-blockers and 5α-reductase inhibitors) versus monotherapy in patients with moderate to severe BPH.
- Key Findings:
- Combination therapy (e.g., tamsulosin + finasteride) was more effective in improving urinary symptoms and flow compared to monotherapy with either treatment alone.
- Combination therapy also reduced the risk of acute urinary retention and BPH-related surgeries.
- Finasteride reduced prostate size, while tamsulosin improved urinary flow.
- Impact: The COMBAT trial reinforced the effectiveness of combining α1-blockers and 5α-reductase inhibitors for improving symptoms, reducing disease progression, and minimizing the need for surgical intervention in BPH.
5. The MTOPS-2 Study (Medical Therapy of Prostatic Symptoms-2)
- Year: 2007
- Purpose: This follow-up study to the MTOPS trial aimed to examine the long-term outcomes and safety of combination therapy.
- Key Findings:
- Results confirmed that combination therapy reduced symptoms and progression of BPH more effectively than monotherapy over long periods.
- There were fewer instances of acute urinary retention and BPH-related surgeries.
- Impact: MTOPS-2 further validated the findings of the original MTOPS trial and solidified the role of combination therapy in the long-term management of BPH.
6. The ALFUZOSIN vs. TERAZOSIN Trial
- Year: 2007
- Purpose: A head-to-head comparison of alfuzosin and terazosin for treating LUTS associated with BPH.
- Key Findings:
- Both drugs were similarly effective in reducing BPH symptoms and improving urinary flow.
- Alfuzosin had a better side-effect profile with fewer cardiovascular events (e.g., postural hypotension).
- Terazosin, while effective, was associated with more frequent side effects such as hypotension and dizziness.
- Impact: This trial helped position alfuzosin as a preferable treatment for many patients with BPH, especially those at risk of cardiovascular events.
7. The MTOPS + FINASTERIDE Study (MTOPS/Finasteride Study)
- Year: 2003
- Purpose: To examine the effects of finasteride in combination with other drugs for BPH management.
- Key Findings:
- Finasteride reduced prostate volume, improved urinary symptoms, and reduced the need for surgery.
- Long-term use led to a significant decrease in the incidence of acute urinary retention and BPH-related surgeries.
- Impact: The study reinforced finasteride’s role as an important treatment for BPH, demonstrating its long-term effectiveness in reducing prostate size and improving urinary symptoms.
8. The ALLHAT Study (Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial)
- Year: 2002
- Purpose: While the study was primarily focused on hypertension, it included a subgroup of BPH patients using doxazosin.
- Key Findings:
- Doxazosin, an α1-blocker, was effective in lowering blood pressure and showed some improvement in urinary symptoms associated with BPH.
- The trial provided evidence for the use of doxazosin in patients with both hypertension and BPH.
- Impact: The ALLHAT trial supported the role of α1-blockers like doxazosin for managing both hypertension and BPH.
9. The REDUCE Trial (Reduction by Dutasteride of Prostate Cancer Events)
- Year: 2010
- Purpose: To evaluate dutasteride, a 5α-reductase inhibitor, for BPH and prostate cancer prevention.
- Key Findings:
- Dutasteride significantly reduced prostate volume and improved urinary symptoms.
- It was associated with a decrease in acute urinary retention and prostate-related surgeries.
- Impact: This trial reinforced the role of 5α-reductase inhibitors like dutasteride in the management of BPH, particularly for patients with larger prostate volumes and at risk for disease progression.
Conclusion of Benign Prostatic Enlargement
While Benign Prostatic Hyperplasia (BPH) is a common and often manageable condition, it can significantly impact a man’s quality of life. Early recognition of symptoms, understanding the difference between BPH and prostate cancer, and exploring treatment options can help men regain control over their health. By adopting a proactive approach to prostate health, men can minimize the impact of prostate enlargement and maintain a good quality of life.


2 Comments