Gastroenterology Treatment for IBS and GERD: Comprehensive Guide for Effective Relief
Introduction:
Gastrointestinal (GI) disorders like Irritable Bowel Syndrome (IBS), Inflammatory Bowel Disease (IBD), and Gastroesophageal Reflux Disease (GERD) can have a profound impact on your health and quality of life. While these conditions share some common symptoms such as abdominal pain, bloating, and digestive disturbances, they are distinct diseases with different causes and treatment approaches. This article explores gastroenterology treatment options for IBS, IBD, and GERD, helping you understand how to manage each condition effectively.
The stomach lining contains several types of cells, each with a unique role in digestion and protection.
Parietal Cells: The Acid Producers
Parietal cells in the stomach are responsible for producing hydrochloric acid (HCl), which plays a crucial role in breaking down food and activating digestive enzymes. These cells also secrete intrinsic factors, which are essential for the absorption of vitamin B12.
- Activation of H+/K+ ATPase Pump: Parietal cells release HCl through the activation of the H+/K+ ATPase pump.
- Stimuli for Acid Production:
- Histamine (via H2 receptors) stimulates this pump to release acid.
- Acetylcholine (via M1 and M3 receptors) also triggers the pump to release acid.
- Gastrin (via CCK receptors) further enhances acid secretion.
Both acetylcholine and gastrin increase acid production by promoting histamine release, which boosts the overall gastric acid secretion.
G Cells: The Gastrin Secretors
G cells are specialized cells located in the stomach lining. They secrete gastrin, a hormone that plays a vital role in stimulating parietal cells to produce more HCl.
- Function of Gastrin: Gastrin promotes gastric motility, ensuring that food moves efficiently through the stomach and digestive system.
- Regulation of Acid Production: Gastrin’s secretion helps regulate the stomach’s acid levels, contributing to effective digestion.
Chief Cells: The Protein Breakdown Helpers
Chief cells are responsible for producing pepsinogen, which is an inactive precursor of the enzyme pepsin.
- Activation of Pepsin: When exposed to stomach acid, pepsinogen is converted into active pepsin, an enzyme that breaks down proteins into smaller peptides, making digestion easier.
- Role in Digestion: Pepsin is crucial for protein digestion in the stomach, helping to initiate the breakdown of food before it enters the small intestine.
Mucus-Secreting Cells: The Protective Barrier
Mucus-secreting cells in the stomach lining release mucus that forms a protective coating over the stomach walls. This mucus plays an important role in safeguarding the stomach from the highly acidic environment.
- Protection from Acid: The mucus layer acts as a barrier, preventing stomach acid from damaging the stomach lining.
- Maintaining Stomach Health: By protecting the stomach lining from the harsh effects of HCl, these cells help maintain the overall health and integrity of the stomach tissue.
1. IBS vs. IBD vs. GERD: What Are the Key Differences?
What is IBS? (Irritable Bowel Syndrome)
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder, meaning it affects how the gut functions but does not cause structural damage to the intestines. IBS is characterized by:
- Abdominal pain or cramping
- Bloating
- based on the Changes in bowel habits IBS is of three types
- BS-D (Diarrhea-predominant): Characterized by frequent diarrhea.
- IBS-C (Constipation-predominant): Involves chronic constipation.
- IBS-M (Mixed): A combination of both diarrhea and constipation.
IBS is typically triggered by stress, dietary factors, or hormonal changes and can cause significant discomfort. However, unlike IBD, IBS does not cause inflammation or damage the gastrointestinal tract.
What is IBD? (Inflammatory Bowel Disease)
Inflammatory Bowel Disease (IBD), on the other hand, refers to a group of chronic inflammatory conditions that cause actual damage to the gastrointestinal tract. The two main types of IBD are:
- Crohn’s Disease: Affects any part of the GI tract, from mouth to anus.
- Ulcerative Colitis: Primarily affects the large intestine (colon) and rectum.
Unlike IBS, IBD is marked by inflammation and can lead to ulcers, bleeding, and tissue damage in the intestines. Common symptoms include:
- Chronic diarrhea
- Abdominal pain
- Blood in stools
- Weight loss and fatigue
IBD often requires more aggressive treatment, including immunosuppressive medications, biological therapies, and in some cases, surgery.
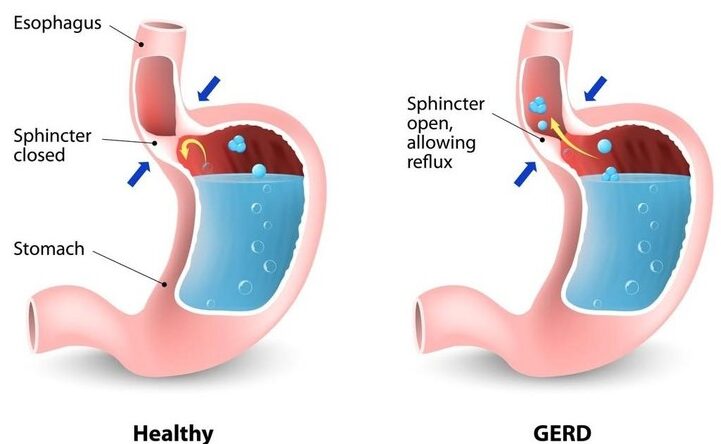
What is GERD? (Gastroesophageal Reflux Disease)
Gastroesophageal Reflux Disease (GERD) is a chronic condition where stomach acid or bile irritates the esophagus, leading to:
- Heartburn (a burning sensation in the chest)
- Regurgitation (acid reflux)
- Difficulty swallowing (dysphagia)
- Chronic cough and hoarseness (in some cases)
- Odynophagia (rare)
Unlike IBS and IBD, GERD primarily affects the esophagus and is related to the malfunction of the lower esophageal sphincter (LES), which fails to prevent acid reflux. GERD can cause significant damage to the esophagus if left untreated and may lead to esophageal ulcers, strictures, or Barrett’s esophagus, a pre-cancerous condition.
Gastroenterology Treatment for IBS and GERD: GERD & IBS management & treatment
Managing Irritable Bowel Syndrome (IBS) and Gastroesophageal Reflux Disease (GERD) together requires a careful, balanced approach. Although they are separate conditions, both can share symptoms like abdominal discomfort, and they are influenced by similar factors, including diet, lifestyle, and stress. Treating both conditions simultaneously can help reduce overlapping symptoms, improve digestion, and enhance overall quality of life.
Why a Dual Approach is Necessary
When IBS and GERD occur together, they can exacerbate each other’s symptoms. For example, acid reflux from GERD can worsen IBS symptoms like bloating, while the gas and bloating from IBS can aggravate acid reflux. By addressing both conditions at the same time, you can prevent this symptom overlap and keep both conditions in check.
The Importance of Consulting a Gastroenterologist
A gastroenterologist can evaluate the severity of each condition and create a personalized treatment plan. They can guide you on how to effectively combine dietary, medical, and lifestyle changes to manage both IBS and GERD together.
2.1 Dietary Treatment for IBS and GERD
Best Foods to Eat:
- Low FODMAP Diet for IBS: FODMAPs (fermentable carbohydrates) are known to trigger IBS symptoms. A low FODMAP diet helps reduce bloating and discomfort for many people with IBS.
- Alkaline Foods for GERD: Foods like leafy greens, cucumbers, and melons are naturally alkaline, which can help neutralize stomach acid and alleviate GERD symptoms.
Foods to Avoid:
- Trigger Foods for IBS: High-fat foods, dairy, and artificial sweeteners can worsen IBS symptoms.
GERD-Specific Triggers:
- Alcohol
- Caffeine
- Tobacco use
- Fatty or fried foods
- Chocolate
- Peppermint
- Spicy foods
- Citrus juices
Meal Timing and Portion Control:
Eating smaller, more frequent meals can reduce symptoms of both IBS and GERD. Large meals can overfill the stomach, increasing the risk of acid reflux and IBS flare-ups.
2.2 Medication Options in Gastroenterology Treatment for IBS and GERD
IBS Medications:
- Antispasmodics: These medications help relieve abdominal cramps by relaxing muscles in the digestive tract.
- Laxatives and Anti-Diarrheal Drugs: These are used depending on the type of IBS (constipation-predominant or diarrhea-predominant).
GERD Medications in Gastroenterology Treatment for IBS and GERD
- Proton Pump Inhibitors (PPIs) reduce stomach acid production and provide long-term relief from GERD symptoms.
- H2 Blockers block histamine receptors in stomach cells, decreasing acid production.
- Antacids neutralize stomach acid and offer quick, short-term relief from acid reflux.
Gastroenterology Treatment for IBS and GERD: A Simple Guide to Antacid Use
Antacids are medications commonly used to neutralize stomach acid, providing relief from symptoms associated with conditions like GERD (Gastroesophageal Reflux Disease), dyspepsia, and peptic ulcers. They work by reducing the acidity in the stomach, offering quick pain relief but do not address the underlying causes of these conditions.
Types of Antacids Used in Gastroenterology Treatment for IBS and GERD
- Systemic Antacids: These are absorbed into the bloodstream and work quickly but aren’t ideal for long-term use. Examples include:
- Sodium citrate

Milk of Magnesia: Magnesium Hydroxide
- Sodium bicarbonate

Rennie: Calcium Carbonate, Magnesium Carbonate
- Magnesium trisilicate
- Aluminum hydroxide gel
- Calcium carbonate
- Magaldrate
- Sodium citrate
Advantages of Nonsystemic Antacids:
- They don’t cause rebound acidity.
- Slower but longer-lasting effects.
- Most combination formulas balance the side effects, such as constipation (from aluminum) and diarrhea (from magnesium).
How Antacids Work
Antacids neutralize stomach acid but do not reduce the amount of acid produced. They provide quick relief from acid-related discomfort by increasing the gastric pH, making the stomach less acidic. However, this may lead to minor, short-lived increases in acid production.


Gaviscon Double Action: Sodium Alginate, Sodium Bicarbonate, Calcium Carbonate

Acidex: Sodium Alginate, Sodium Bicarbonate, Calcium Carbonate

Gaviscon Advance Sodium Alginate, Potassium Bicarbonate

Peptac: Sodium Alginate, Sodium Bicarbonate, Calcium Carbonate
Product | Key Ingredients | Purpose |
Milk of Magnesia | Magnesium Hydroxide | Antacid and laxative |
| Rennie | Calcium Carbonate, Magnesium Carbonate | Neutralizing antacid |
Acidex | Sodium Alginate, Sodium Bicarbonate, Calcium Carbonate | Barrier and neutralizing antacid |
Peptac | Sodium Alginate, Sodium Bicarbonate, Calcium Carbonate | Barrier and neutralizing antacid |
Gaviscon | Sodium Alginate, Sodium Bicarbonate, Calcium Carbonate | Barrier and neutralizing antacid |
Gaviscon Advance | Sodium Alginate, Potassium Bicarbonate | Enhanced barrier for severe acid reflux |
Gaviscon Double Action | Sodium Alginate, Sodium Bicarbonate, Calcium Carbonate | Dual-action for fast relief |
Combining Antacids with Other Medications
Some antacid formulations include simethicone, which helps reduce gas and bloating, and alginates, which protect the esophagus from acid reflux. Combining different types of antacids (such as aluminum hydroxide with magnesium hydroxide) can offer rapid and sustained relief without major side effects.
Risks and Considerations
- Milk-Alkali Syndrome: Overusing calcium carbonate or sodium bicarbonate, especially with calcium-rich foods like milk, can lead to hypercalcemia, renal insufficiency, and metabolic alkalosis.
- Drug Interactions: Antacids can affect the absorption of other medications, especially those that rely on an acidic environment for proper absorption, such as tetracycline antibiotics. It’s recommended to take antacids 2-3 hours apart from other medications to avoid interactions.
- Aluminum Compounds: These can adsorb other drugs and form insoluble complexes that cannot be absorbed, reducing the effectiveness of certain treatments.
When to Use Antacids
Antacids are typically taken between meals and at bedtime when symptoms of gastric hyperacidity are most common. Liquid preparations tend to be more effective than tablets, and antacids with longer-lasting effects may be preferred for chronic conditions.
Conclusion
In the context of gastroenterology treatment for IBS and GERD, antacids can provide short-term relief from discomfort caused by excess stomach acid. However, they should be used cautiously and as part of a broader treatment plan that may include dietary changes, lifestyle adjustments, and medications. Consult a gastroenterologist for a tailored treatment strategy to manage IBS and GERD effectively.
H2 Receptor Antagonists: Overview and Mechanism of Action in Gastroenterology Treatment for IBS and GERD
H2 receptor antagonists are medications that block histamine from binding to H2 receptors on the stomach’s parietal cells, which reduces acid production. These drugs are effective in treating conditions like GERD, Peptic Ulcer Disease (PUD), Zollinger-Ellison Syndrome (ZES), and stress-induced ulcers.
Common H2 Blockers & Available Brands
- Cimetidine – Tagamet, Tagamet HB
- Ranitidine – Zantac, Rantac, Aciloc, Zinetac
- Famotidine – (Most potent) – Pepcid, Pepcid AC, Famocid
- Roxatidine – Roxane, Roxitac, Rox
- Nizatidine – Axid, Tazac, Nizax
- Loxatidine – Though not as commonly marketed globally, it may be found under regional or generic names.
How H2 Blockers Work
These drugs work by inhibiting histamine at the H2 receptors, primarily reducing basal (nocturnal) acid secretion. They are less effective against acid secretion triggered by gastrin or acetylcholine (ACh). This mechanism helps lower overall stomach acidity, making them effective in managing acid-related disorders.
Clinical Uses
H2 blockers are used to treat:
- GERD: Reduces acid reflux and its symptoms.
- PUD: Promotes ulcer healing.
- ZES: Reduces excessive acid production.
- Stress Ulcers: Prevents ulcers due to physical stress.
Side Effects and Drug-Specific Notes
- Cimetidine: Known for several side effects such as:
- Crossing the blood-brain barrier, potentially causing mental confusion.
- Inhibiting dihydrotestosterone, leading to impotence.
- Long-term use may cause gynecomastia (increased breast tissue in men) and galactorrhea (milk production in women).
- It can interact with liver enzymes, increasing levels of drugs like warfarin and theophylline.
- Famotidine: The most potent H2 blocker with fewer side effects compared to cimetidine. Does not affect androgen receptors or liver enzymes.
- Nizatidine: It has negligible first-pass metabolism, meaning nearly all of the dose reaches the bloodstream, with 100% bioavailability.
- Loxatidine: A non-competitive H2 blocker with a different mechanism from other H2 blockers.
Effects on Gastric Acid Secretion
H2 blockers inhibit acid secretion across all phases (basal, psychic, neurogenic, gastric) with the most significant effect on nocturnal acid secretion. They reduce gastric acid, pepsin, and intrinsic factor secretion but do not affect vitamin B12 absorption. These drugs promote ulcer healing and prevent stress ulcers.
Conclusion
H2 receptor antagonists are still useful in treating acid-peptic diseases like GERD, ulcers, and stress ulcers, though newer medications like proton pump inhibitors (PPIs) have largely replaced them. Some side effects, especially with cimetidine, limit their use, but these drugs remain an important option for certain patients.
2. Proton Pump Inhibitors (PPIs)
“The treatment of GERD, as outlined by the American College of Gastroenterology (ACG) guidelines, recommends proton pump inhibitors (PPIs) as the first-line therapy for chronic acid reflux. Clinical evidence from recent studies supports the efficacy of PPIs in reducing esophageal inflammation and preventing complications like Barrett’s esophagus.”
Proton Pump Inhibitors (PPIs) are considered the most potent and effective drugs for reducing gastric acid secretion. Proton Pump Inhibitors (PPIs) – MOA– irreversibly inhibit the H+/K+ ATPase enzyme in the parietal cells of the stomach, which is responsible for producing gastric acid. Some common PPIs include:
- Omeprazole – Prilosec, Losec, Omez
- Esomeprazole – Nexium, Nexpro, Esomac, Essocam
- Pantoprazole – Protonix, Pantocid, Pantoloc, Pan
- Lansoprazole – Prevacid, Lanzol, Agopton, Zoton, Lanzor
- Rabeprazole – Aciphex, Pariet, Rabicip, Rablet
- Dexrabeprazole – Dexilant, Dexrab
How PPIs Work:
PPIs are prodrugs that are activated in the acidic environment of the stomach. They are typically administered in enteric-coated formulations to prevent them from being broken down by stomach acid. After absorption, they reach the parietal cells, where the active form of the drug irreversibly blocks the proton pump, reducing acid secretion. PPIs can inhibit both basal (nighttime) and stimulated acid production (triggered by food or other factors).
Indications for PPIs:
- Peptic Ulcer Disease (PUD): Effective for ulcers caused by NSAIDs or other factors.
- GERD: Reduces acid reflux and alleviates symptoms.
- Zollinger-Ellison Syndrome (ZES): Manages excessive acid production.
- Stress Ulcers: In patients at risk of gastric bleeding due to stress.
PPIs are usually taken in the morning before breakfast on an empty stomach. They have a short half-life but provide prolonged acid suppression (up to 24 hours). Pantoprazole, esomeprazole, and lansoprazole can also be administered intravenously for quicker action, especially in hospitalized patients.
Side Effects and Considerations:
- Common Side Effects: Diarrhea, headache, and abdominal pain.
- Long-Term Risks: Prolonged use of PPIs has been linked to reduced vitamin B12 absorption, increasing the risk of hip fractures due to impaired calcium absorption, and higher susceptibility to infections like Clostridium difficile and pneumonia.
Despite these risks, PPIs are still the first-line treatment for acid-related disorders, including GERD and PUD.
3. Anticholinergic Drugs
Anticholinergic agents like Pirenzepine, Propantheline, and Oxyphenonium work by blocking the action of acetylcholine (ACh) on muscarinic receptors in the stomach, reducing gastric acid secretion. These drugs are less commonly used than PPIs or H2 blockers due to their side effects, which may include dry mouth, blurred vision, and urinary retention.
4. Prostaglandin Analogue
Misoprostol is a prostaglandin analog used to protect the gastric mucosa. It promotes mucus and bicarbonate production, thereby protecting the stomach lining from the erosive effects of gastric acid. Misoprostol is primarily used in preventing NSAID-induced ulcers but can cause side effects like diarrhea and abdominal cramps.
5. Mucosal Protectants
Mucosal protectants are used to help heal and protect the gastric lining, particularly in patients with ulcers. These drugs form protective barriers over the ulcerated areas, allowing healing to occur. Common mucosal protectants include:
- Sucralfate: Forms a viscous gel that adheres to ulcer sites, promoting healing and preventing further damage.
- Bismuth Subsalicylate (tri potassium dicitratobismuthate): Has an antibacterial effect, particularly useful in eradicating Helicobacter pylori infections.
Other mucosal protectants like carbenoxolone (a derivative of liquorice) stimulate the production of protective mucus in the stomach, offering additional support in healing gastric ulcers.
Conclusion
In summary, various drug classes are available to manage conditions associated with excessive gastric acid production. Proton pump inhibitors (PPIs) are the most effective for long-term acid suppression and are the treatment of choice for many acid-related disorders, including GERD, PUD, and ZES. H2 blockers also reduce acid secretion but are generally less effective than PPIs. Meanwhile, anticholinergic drugs and prostaglandin analogs play supportive roles in reducing gastric acid or protecting the mucosal lining.
While these treatments are generally safe, long-term use of PPIs should be carefully monitored due to potential side effects, including nutrient malabsorption and an increased risk of certain infections. Always consult with a healthcare provider to determine the best treatment plan for your condition.
Medications for Combined Treatment:
A gastroenterologist may suggest a combination of medications to manage both conditions while minimizing any potential interactions. They will monitor for side effects and adjust dosages to ensure both IBS and GERD are effectively controlled.
2.3 Natural / home Remedies for Dyspepsia / Heartburn and Lifestyle Adjustments in Gastroenterology Treatment for IBS and GERD
Probiotics for IBS:
Probiotics can help restore a healthy balance of gut bacteria, which may reduce symptoms like bloating and irregular bowel movements in people with IBS.
Managing GERD Naturally:
- Elevating the head of your bed can help prevent nighttime acid reflux.
- Avoid lying down immediately after meals to reduce the chances of acid reflux.
- Reducing the body weight if possible
Lifestyle Changes:
- Stress Management: Techniques such as meditation, yoga, and deep breathing can help reduce stress, which is a known trigger for both IBS and GERD.
- Regular Exercise: Physical activity promotes digestion and reduces stress, which can improve symptoms of both conditions.
Summary of Heartburn, Indigestion, and Dyspepsia Remedies During Pregnancy
- Eat Smaller, More Frequent Meals
- Reduce meal size to avoid pressure on the stomach and prevent discomfort.
- Avoid Trigger Foods
- Steer clear of spicy, fatty, and acidic foods, chocolate, caffeine, and citrus.
- Stay Upright After Eating
- Remain upright for at least an hour to prevent acid reflux.
- Drink Herbal Teas
- Ginger and chamomile teas can help soothe digestive discomfort (ensure they are pregnancy-safe).
- Drink Plenty of Water
- Stay hydrated to prevent constipation, but avoid large amounts during meals.
- Baking Soda Water for Relief
- Occasionally mix half a teaspoon of baking soda in water to neutralize stomach acid.
- Elevate Your Head While Sleeping
- Use pillows to raise the head of your bed and reduce acid reflux at night.
- Chew Sugar-Free Gum
- Gum increases saliva production, which helps neutralize stomach acid.
- Practice Relaxation Techniques
- Stress management through deep breathing, yoga, or meditation can improve digestion.
- Wear Loose Clothing
- Avoid tight clothes to reduce pressure on the stomach and ease digestion.
When to Consult a Doctor:
- If symptoms are severe or persistent.
- If there is blood in stool or vomit.
- If experiencing weight loss, difficulty swallowing, or food getting stuck.
These tips provide safe, natural ways to manage heartburn and indigestion during pregnancy. Always consult a healthcare provider before making significant changes.
3. How to Reduce Symptoms and Prevent Flare-Ups of IBS and GERD
Identifying Triggers:
Keep a food and symptom diary to track specific foods or situations that worsen your symptoms. This makes it easier to avoid triggers and manage flare-ups.
Preventative Measures:
Being consistent with dietary changes, such as following a low FODMAP diet for IBS or avoiding acidic foods for GERD, can help prevent flare-ups and reduce discomfort.
Long-Term Management Strategies:
Work with your healthcare provider to develop a sustainable treatment plan that includes a tailored diet, medications, and lifestyle changes to manage both conditions over time.
4. When to See a Gastroenterologist for Gastroenterology Treatment for IBS and GERD
Warning Signs:
If your symptoms become more severe, more frequent, or don’t improve with treatment, it’s important to see a gastroenterologist. Other warning signs include difficulty swallowing, unexplained weight loss, or blood in your stool.
Advanced Treatment Options in Gastroenterology Treatment for IBS and GERD:
Your gastroenterologist might recommend further diagnostic tests, like an endoscopy, to assess any damage caused by acid reflux or to explore other underlying causes of your symptoms.
Surgical Options:
For severe GERD that doesn’t respond to other treatments, procedures like fundoplication may be considered.
5. Conclusion: Finding Relief with Gastroenterology Treatment for IBS and GERD
It is possible to manage both IBS and GERD effectively with the right approach. A combination of dietary changes, medication, and lifestyle adjustments tailored to your specific needs can make a significant difference in symptom control. Consulting a gastroenterologist is key to developing a treatment plan that improves your long-term quality of life and helps you manage both conditions more effectively.
6. Frequently Asked Questions (FAQ) in Gastroenterology Treatment for IBS and GERD
Can IBS and GERD be treated together?
Yes, with a customized plan that includes dietary adjustments, medications, and lifestyle changes, both conditions can be managed together.
What is the best diet for IBS and GERD sufferers?
A low FODMAP diet for IBS and alkaline foods for GERD are beneficial. Additionally, avoiding trigger foods for each condition is important.
Are there any natural remedies for IBS and GERD?
Probiotics may help manage IBS symptoms while elevating the head of your bed and avoiding lying down after meals can help reduce GERD symptoms.
What medications are most effective for both IBS and GERD?
For IBS, antispasmodics, laxatives, and anti-diarrheal may be used. For GERD, PPIs, H2 blockers, and antacids are common treatments.
Can stress worsen IBS and GERD symptoms?
Yes, stress is a known trigger for both IBS and GERD. Stress management techniques like meditation, yoga, and deep breathing can be very helpful in controlling symptoms.
References:
“For further reading on the management of GERD, refer to the latest guidelines provided by the American Gastroenterological Association (AGA) You can also access additional clinical studies on IBS and GERD treatment through PubMed“
“The information provided in this article is for general educational purposes only. It is not a substitute for medical advice. Please consult with a healthcare provider or gastroenterologist for a personalized treatment plan tailored to your needs.”



Leave a Reply